Context & Role
As Principal UX Product Designer at Florida Blue, I led the redesign of a complex legacy claims inventory and listing system critical to auditors and support staff. My responsibilities included managing the UX team, conducting research, and overseeing the full design lifecycle from concept through delivery.
The Challenge
The legacy claims system was fragmented across multiple disconnected tools, leading to inefficiencies, increased errors, and user frustration. It also lacked proper data segmentation needed for HIPAA compliance. Auditors and support staff struggled with time-consuming navigation and inconsistent data views, impacting productivity and accuracy.
Tools
- Figma and Adobe XD
- Microsoft Teams
- Google Sheets
- Figjam
Research & Insights
I conducted virtual shadowing sessions and interviews with claims staff to understand workflows, pain points, and compliance needs. Collaborating with Business Systems Analysts and stakeholders, we identified core issues and translated them into clear user stories and design requirements.
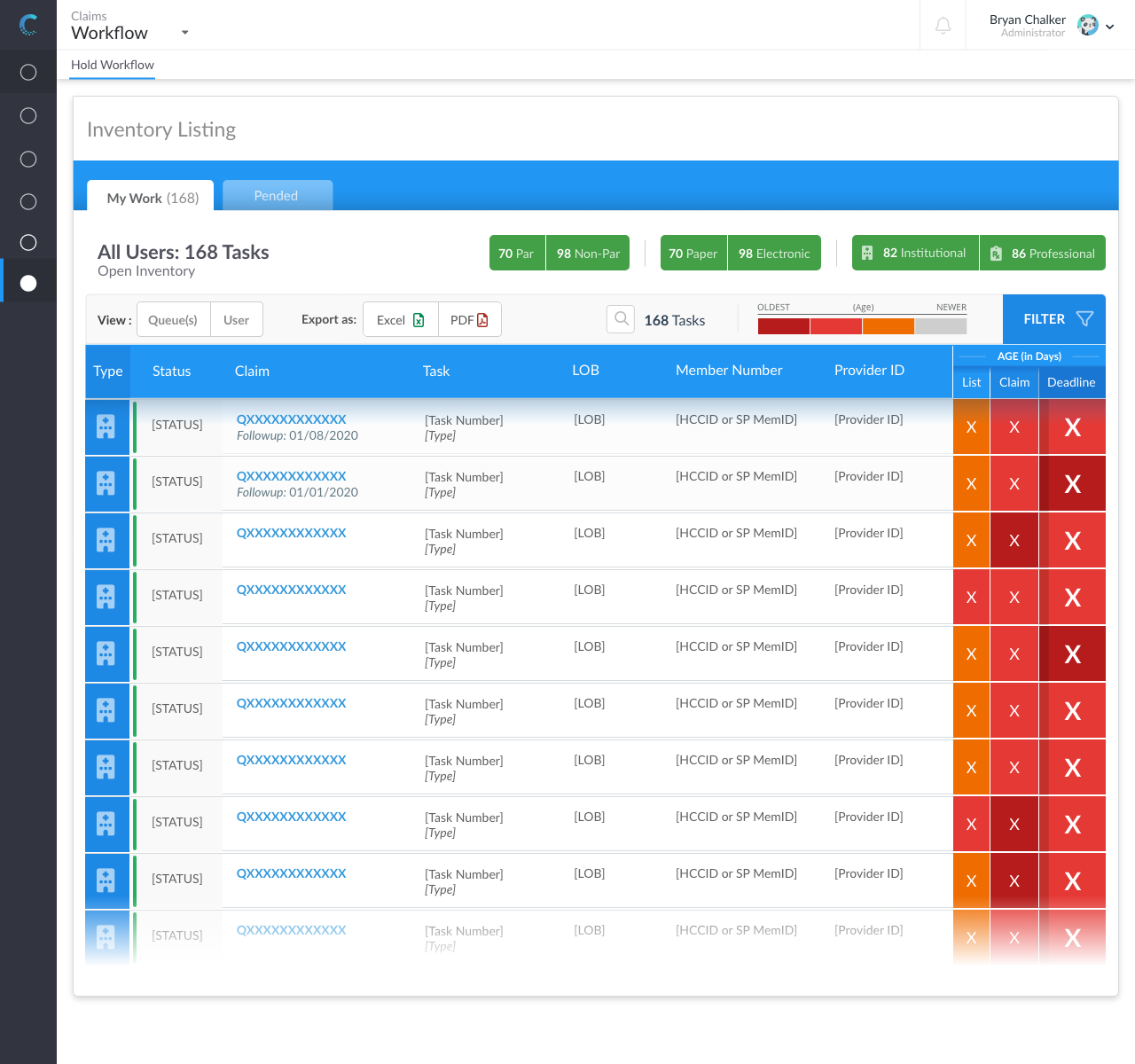
Design Approach & Solutions
Leading a UX team, I designed Claims Connect—a centralized, role-based web platform consolidating all claims data into a single interface. We implemented dual data views and smart inventory filters to reduce cognitive load and streamline navigation. Using Figma and Adobe XD, we developed interactive prototypes and conducted usability testing, iterating based on user feedback and analytics. Design tokens ensured consistent UI and smooth developer handoff.
Impact & Results
The redesigned platform significantly improved efficiency, reducing navigation time and errors for auditors and support staff. It ensured strict HIPAA and PHI compliance while increasing user satisfaction. The solution unified disparate data sources, enabling faster, more accurate claims processing.
Learnings & Next Steps
This project reinforced the importance of deep user research in regulated environments and close collaboration between UX, development, and business teams. Future enhancements include advanced analytics and automation to further support claims workflows.